Nankai University Research Team Achieves New Advances in Intelligent Assessment of Parkinson’s Disease
A research team led by Professors Huo Weiguang and Han Jianda from the College of Artificial Intelligence at Nankai University, in collaboration with researchers from Tianjin Huanhu Hospital, City St George’s, University of London, and Imperial College London, has published a study in npj Digital Medicine, a leading journal in the field of digital medicine. The study is titled “Deep Learning-enabled Accurate Assessment of Gait Impairments in Parkinson's Disease Using Smartphone Videos”.
The study proposes an innovative deep learning framework that enables precise quantitative assessment of gait impairment severity in Parkinson’s disease (PD) and accurate assessment of subtle medication effects that are difficult to capture with traditional clinical scales, such as the UPDRS, using only smartphone-recorded walking videos. The team further identified multiple novel digital biomarkers highly responsive to disease progression and medication effects using this framework.
Figure 1: intelligent assessment of gait impairments in Parkinson’s disease using smartphone videos
The research team developed a novel twin contrast network architecture (Figure 2). By emulating clinicians' assessment process, the model integrates gait videos captured from left and right perspectives with a single camera during patients’ round-trip walking, enabling accurate extraction of motion features and comparative analysis of full-body motion. Unlike conventional approaches that focus solely on predefined clinical gait parameters, the proposed interpretable framework is capable of extracting both conventional gait metrics and previously unexplored digital biomarkers. The model’s performance was validated on a dataset comprising 118 participants, including 87 PD patients and 31 healthy controls.
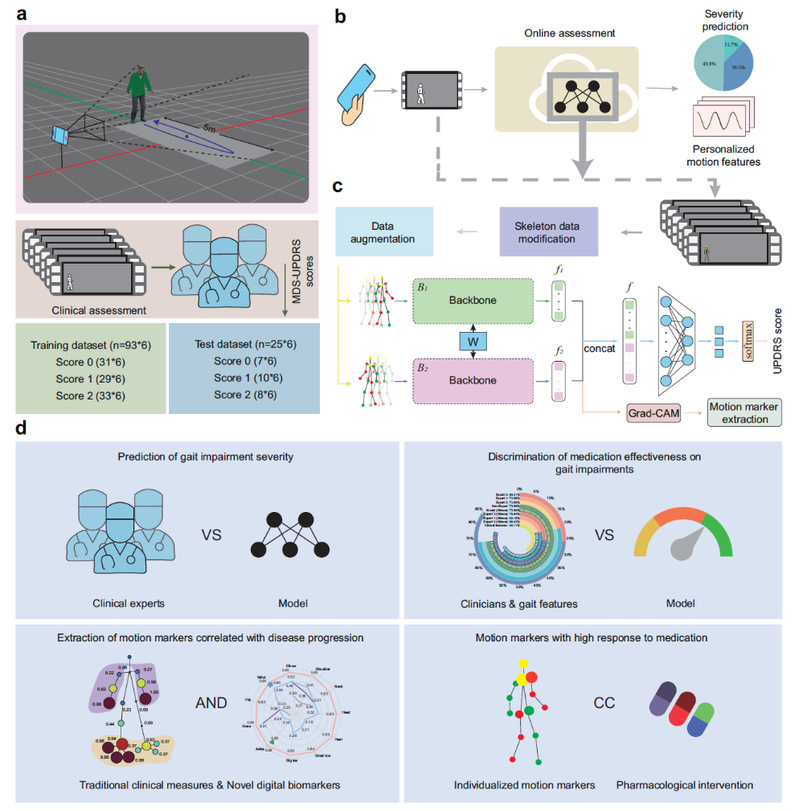
Figure 2: AI-based assessment framework for gait impairments in Parkinson’s disease using smartphone videos
In assessing gait impairment severity, clinical tests on an independent test set (25 participants) demonstrated that the AI model performed comparably to clinical experts. The model achieved an F1 score of 0.806, which is close to the average score of three clinicians (0.819). Its assessment error rate (0.20) was also nearly identical to the clinicians’ average error rate (0.19) (Figure 3).
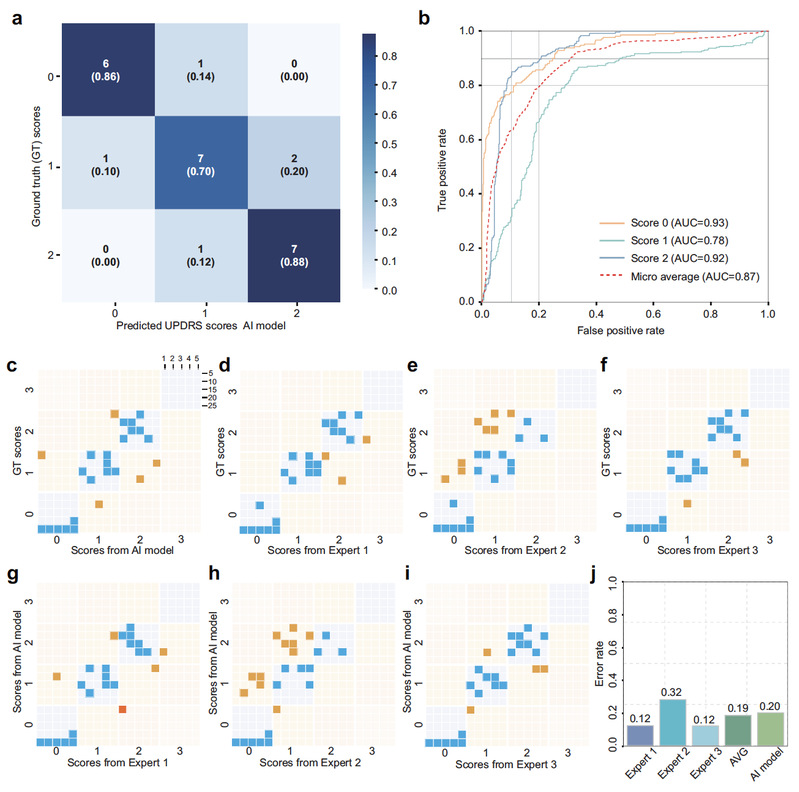
Figure 3: assessment performance between the AI model and clinical experts
To assess medication-induced changes in gait impairments, the AI model overcame the resolution limitations of the UPDRS scale. Medication ON–OFF tests were conducted on 19 PD patients. The model achieved an accuracy of 73.68% in fine-grained evaluation of gait-related medication effects, including those associated with drugs such as Madopar. Notably, within the subgroup of patients whose UPDRS Part III–Gait scores remained unchanged during the medication ON phase (the SwoC cohort), the AI model successfully detected subtle changes in gait impairments that were not reflected by the UPDRS, achieving an accuracy of 66.67%, comparable to the performance of a non-expert clinician (Figure 4).
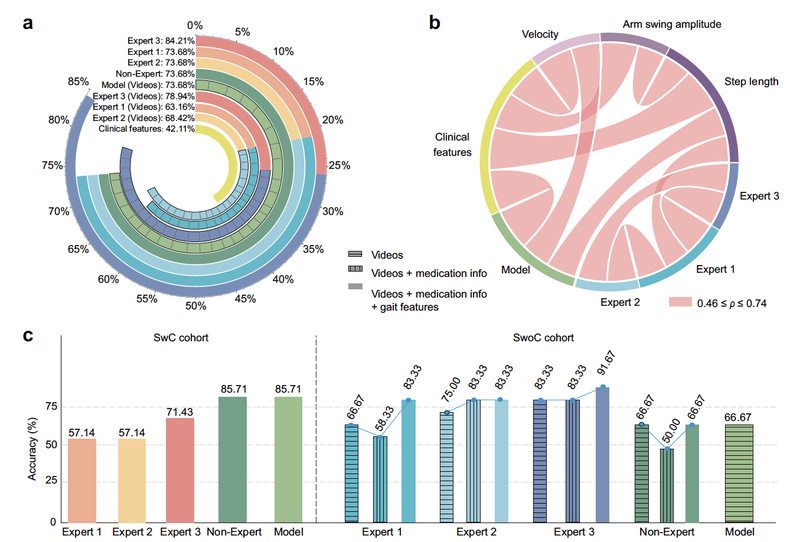
Figure 4: Performance of the AI model in assessing medication effects
In discovering digital biomarkers for Parkinson’s disease gait impairment, the team utilized the proposed interpretable framework to extract multiple novel digital biomarkers that are more sensitive to disease progression and medication response. For example, the study found that the average linear velocity of the ankle joint is more sensitive in reflecting disease severity than traditional arm swing amplitude. In medication ON-OFF tests, 63.16% of patients showed significant differences in new biomarker indicators (e.g., linear acceleration of the neck and head), whereas only 42.11% exhibited significant changes in traditional movement biomarkers (Figure 5).
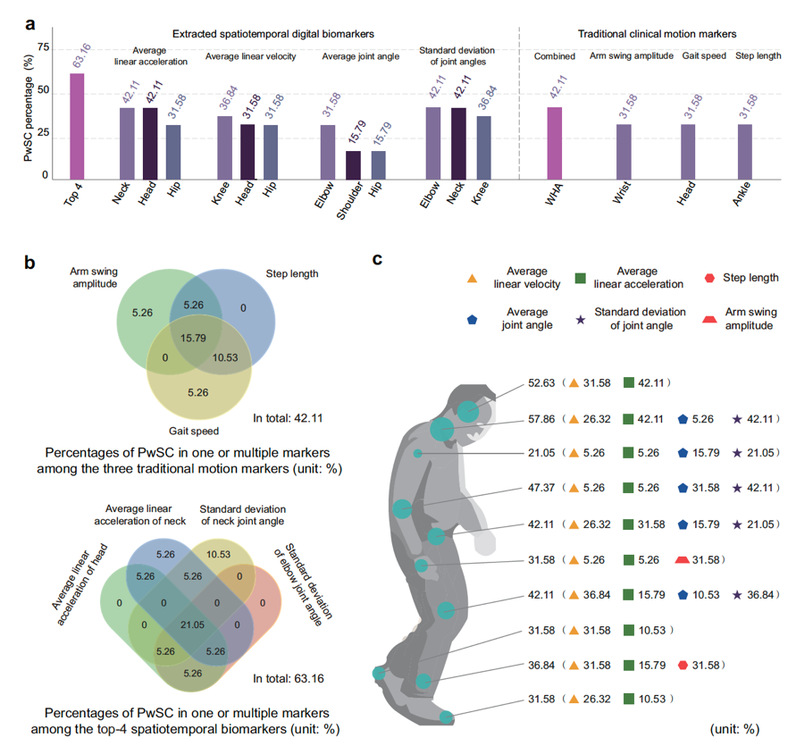
Figure 5: highly responsive digital biomarkers extracted by the AI model
The study demonstrated the potential for convenient, accurate, intelligent at-home diagnosis of Parkinson’s disease, while providing an effective feedback tool for developing personalized treatment plans. The research team has developed an online assessment system, FAGI-PD (https://gaitanalysis.simplaj.fun), based on this framework, designed to assist physicians in achieving remote, precise at-home diagnosis and treatment of Parkinson’s disease. This framework also provides new insights for assessing other neurodegenerative diseases with similar motor impairments, such as stroke and Alzheimer’s disease.
(Edited and translated by Nankai News Team.)









